California must repay $52.7 million to the federal government after incorrectly claiming Medicaid reimbursements.
The repayments are for services provided to “noncitizens with unsatisfactory immigration status,” according to the Department of Health & Human Services Office of Inspector General. This issue came to light following an in-depth review of the payments made between October 1, 2018, and June 30, 2019.
Investigation Exposes Overpayments

A deep dive by the Office of Inspector General into California’s Medicaid claims practices uncovered the misuse of outdated calculations to determine costs for non-emergency services to ineligible recipients.
This misstep cost the state millions, highlighting a severe oversight in financial governance.
Immigration Issues Come to a Head

Amidst an already heated debate on immigration, California’s financial misstep adds fuel to the fire.
Last year’s encounters with nearly 2.5 million suspected illegal migrants marked a new challenge for border control and now, financial management.
Biden Steps In as Migrant Numbers Climb

With migrant interactions at an all-time high, President Biden recently halted asylum processing at non-port entries for numbers surpassing 2,500 a day.
This temporary measure is Biden’s strategy to better manage the influx, spotlighting the administration’s proactive stance on a growing concern.
Stringent Medicaid Rules Highlighted

Federal laws are clear: Medicaid funds for non-citizens are generally off-limits unless it’s an emergency.
California’s mismanagement underlines the critical need for strict compliance with these regulations to prevent financial waste and misuse of federal resources.
Outdated Methods, Costly Results

Investigators pinpointed the root of the problem.
They explained, “California improperly claimed $52.7 million in Federal Medicaid reimbursement because it continued to use the proxy percentage that was developed in the early 2000s without assessing whether the percentage correctly accounted for the costs of providing nonemergency services to noncitizens with UIS [non-citizens with unsatisfactory immigration status] under managed care.”
Oversight Failures

The probe also discovered a significant oversight: “California did not have any policies and procedures for assessing and periodically reassessing the proxy percentage.”
This lapse contributed to the financial mishap, revealing gaps in the state’s regulatory framework.
Call for Refunds and Revisions

The investigation resulted in a strict recommendation from the Office of Inspector General for California to repay the $52.7 million misclaimed.
Additionally, it urged the state to reassess its payment protocols for noncitizens.
A Push for Better Oversight

Further to their findings, authorities have called on California to work with federal agencies to determine the full extent of the misclaimed funds.
This move is aimed at ensuring future compliance and preventing recurrence of such costly errors.
State Admits Fault

In response to the findings, the California Department of Health Care Services did not dispute the audit results.
They’ve agreed to the terms set forth and plan to make the repayment by the end of June, indicating a readiness to resolve the issue swiftly.
How California Will Pay Back

Given the complexities involved in recalculating the payments, California has opted for a manual process to refund the money.
This approach is expected to align with federal guidelines and ensure the accurate return of funds.
Financial Woes Deepen for California
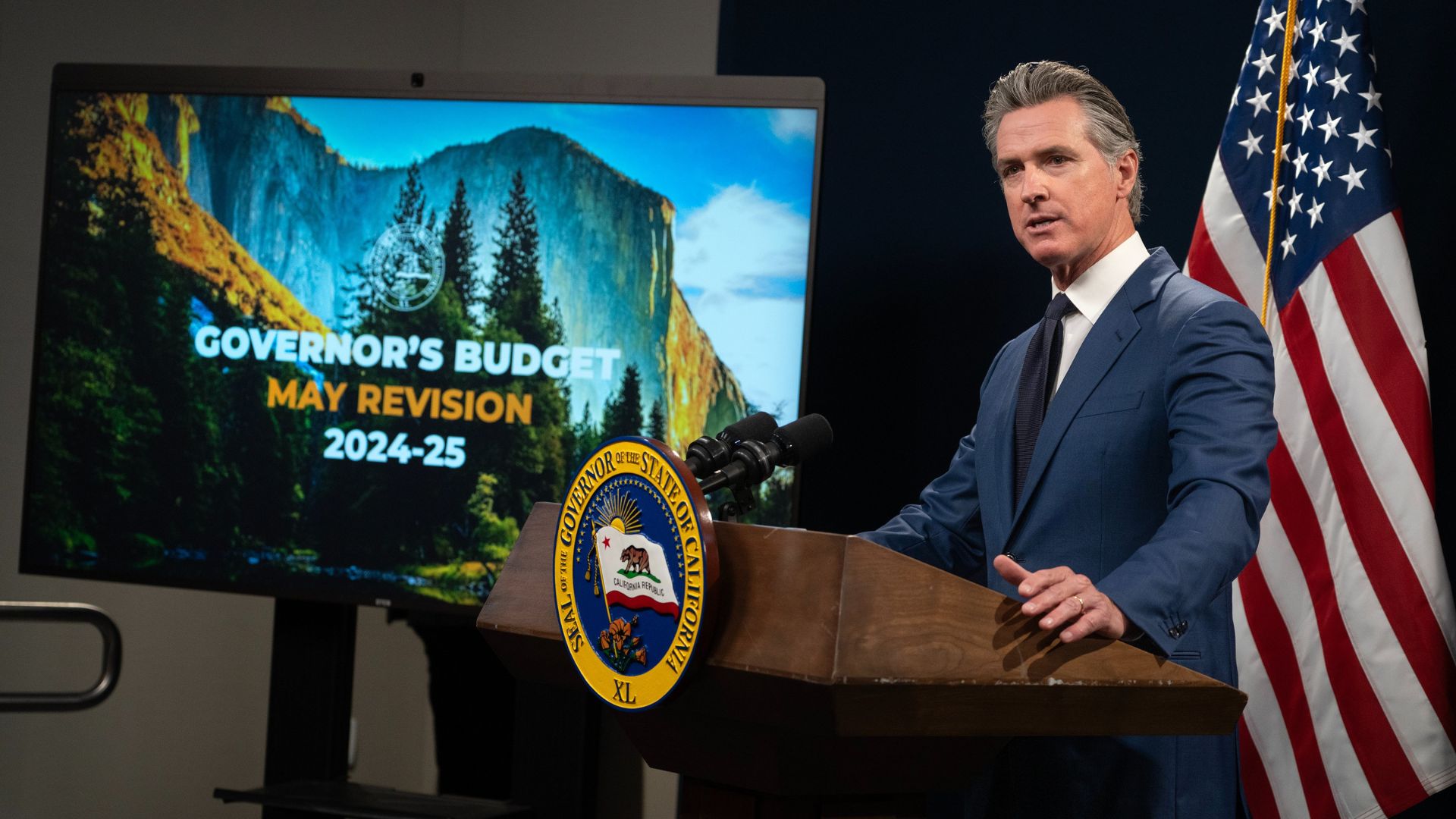
This $52.7 million repayment is just one of many financial hurdles for California.
With a budget deficit potentially escalating to $45 billion due to accumulated spending commitments, the state faces a daunting task of financial restructuring in the midst of managing substantial fiscal deficits.
